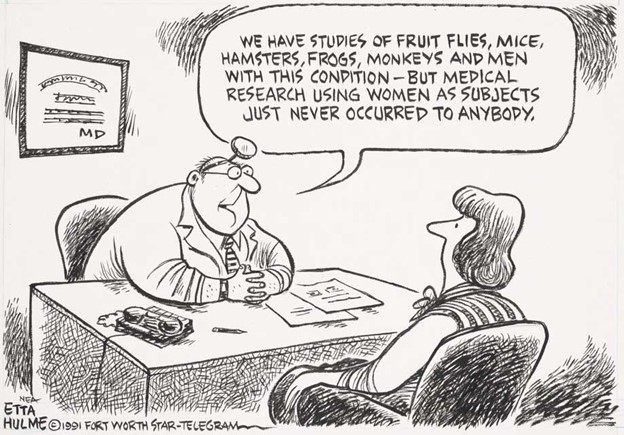
In the past, scientists assumed that males and females were so much alike that the results of studies done on men applied to women as well. They don’t. For this article, journalist Judith Graham asked top doctors and medical researchers what studies need to be done now and what treatments should change. KFF Health News posted her article on June 18, 2024. It also ran in the Washington Post. Funding from the Silver Century Foundation helps KFF Health News develop articles (like this one) on longevity and related health and social issues.
Medical research has shortchanged women for decades. This is particularly true of older women, leaving physicians without critically important information about how to best manage their health.
Late last year, the Biden administration promised to address this problem with a new effort called the White House Initiative on Women’s Health Research. That inspires a compelling question: What priorities should be on the initiative’s list when it comes to older women?
Stephanie Faubion, MD, director of the Mayo Clinic’s Center for Women’s Health, launched into a critique when I asked about the current state of research on older women’s health. “It’s completely inadequate,” she told me.
One example: many drugs widely prescribed to older adults, including statins for high cholesterol, were studied mostly in men, with results extrapolated to women.
“It’s assumed that women’s biology doesn’t matter and that women who are premenopausal and those who are postmenopausal respond similarly,” Faubion said.
“This has got to stop: the FDA has to require that clinical trial data be reported by sex and age for us to tell if drugs work the same, better or not as well in women,” Faubion insisted.
Women who have heart disease are undertreated, compared to men.
Consider the Alzheimer’s drug Leqembi, approved by the FDA last year after the manufacturer reported a 27 percent slower rate of cognitive decline in people who took the medication. A supplementary appendix to a Leqembi study published in the New England Journal of Medicine revealed that sex differences were substantial—a 12 percent slowdown for women, compared with a 43 percent slowdown for men—raising questions about the drug’s effectiveness for women.
This is especially important because nearly two-thirds of older adults with Alzheimer’s disease are women. Older women are also more likely than older men to have multiple medical conditions, disabilities, difficulties with daily activities, auto-immune illnesses, depression and anxiety, uncontrolled high blood pressure and osteoarthritis, among other issues, according to scores of research studies.
Even so, women are resilient and outlive men by more than five years in the United States. As people move into their 70s and 80s, women outnumber men by significant margins. If we’re concerned about the health of the older population, we need to be concerned about the health of older women.
As for research priorities, here’s some of what physicians and medical researchers suggested.
Heart Disease
Why is it that women with heart disease, which becomes far more common after menopause and kills more women than any other condition—are given less recommended care than men?
“We’re notably less aggressive in treating women,” said Martha Gulati, MD, director of preventive cardiology and associate director of the Barbra Streisand Women’s Heart Center at Cedars-Sinai, a health system in Los Angeles. “We delay evaluations for chest pain. We don’t give blood thinners at the same rate. We don’t do procedures like aortic valve replacements as often. We’re not adequately addressing hypertension.
“We need to figure out why these biases in care exist and how to remove them.”
Gulati also noted that older women are less likely than their male peers to have obstructive coronary artery disease—blockages in large blood vessels—and more likely to have damage to smaller blood vessels that remains undetected. When they get procedures such as cardiac catheterizations, women have more bleeding and complications.
What are the best treatments for older women given these issues? “We have very limited data. This needs to be a focus,” Gulati said.
Brain Health
How can women reduce their risk of cognitive decline and dementia as they age?
“This is an area where we really need to have clear messages for women and effective interventions that are feasible and accessible,” said JoAnn Manson, MD, chief of the Division of Preventive Medicine at Brigham and Women’s Hospital in Boston and a key researcher for the Women’s Health Initiative, the largest study of women’s health in the United States.
Numerous factors affect women’s brain health, including stress—dealing with sexism, caregiving responsibilities and financial strain—which can fuel inflammation. Women experience the loss of estrogen, a hormone important to brain health, with menopause. They also have a higher incidence of conditions with serious impacts on the brain, such as multiple sclerosis and stroke.
“Alzheimer’s disease doesn’t just start at the age of 75 or 80,” said Gillian Einstein, PhD, the Wilfred and Joyce Posluns Chair in Women’s Brain Health and Aging at the University of Toronto. “Let’s take a life-course approach and try to understand how what happens earlier in women’s lives predisposes them to Alzheimer’s.”
Mental Health
What accounts for older women’s greater vulnerability to anxiety and depression?
Studies suggest a variety of factors, including hormonal changes and the cumulative impact of stress. In the journal Nature Aging, Paula Rochon, MD, a professor of geriatrics at the University of Toronto, also faulted “gendered ageism,” an unfortunate combination of ageism and sexism, which renders older women “largely invisible,” in an interview in Nature Aging.
Helen Lavretsky, MD, a professor of psychiatry at UCLA and past president of the American Association for Geriatric Psychiatry, suggests several topics that need further investigation. How does the menopausal transition impact mood and stress-related disorders? What nonpharmaceutical interventions can promote psychological resilience in older women and help them recover from stress and trauma? (Think yoga, meditation, music therapy, tai chi, sleep therapy and other possibilities.) What combination of interventions is likely to be most effective?
Cancer
How can cancer screening recommendations and cancer treatments for older women be improved?
Supriya Gupta Mohile, MD, director of the Geriatric Oncology Research Group at the Wilmot Cancer Institute at the University of Rochester, wants better guidance about breast cancer screening for older women, broken down by health status. Currently, women 75 and older are lumped together even though some are remarkably healthy and others, notably frail.
Recently, the U. S. Preventive Services Task Force noted “the current evidence is insufficient to assess the balance of benefits and harms of screening mammography in women 75 years or older,” leaving physicians without clear guidance. “Right now, I think we’re underscreening fit older women and overscreening frail older women,” Mohile said.
The doctor also wants more research about effective and safe treatments for lung cancer in older women, many of whom have multiple medical conditions and functional impairments. The age-sensitive condition kills more women than breast cancer.
“For this population, it’s decisions about who can tolerate treatment based on health status and whether there are sex differences in tolerability for older men and women that need investigation,” Mohile said.
Bone Health, Functional Health and Frailty
How can older women maintain mobility and preserve their ability to take care of themselves?
Osteoporosis, which causes bones to weaken and become brittle, is more common in older women than in older men, increasing the risk of dangerous fractures and falls. Once again, the loss of estrogen with menopause is implicated.
“This is hugely important to older women’s quality of life and longevity, but it’s an overlooked area that is understudied,” said Manson of Brigham and Women’s.
Jane Cauley, DrPH, a distinguished professor at the University of Pittsburgh School of Public Health who studies bone health, would like to see more data about osteoporosis among older Black, Asian and Hispanic women, who are undertreated for the condition. She would also like to see better drugs with fewer side effects.
Marcia Stefanick, PhD, a professor of medicine at Stanford University School of Medicine, wants to know which strategies are most likely to motivate older women to be physically active. And she’d like more studies investigating how older women can best preserve muscle mass, strength and the ability to care for themselves.
“Frailty is one of the biggest problems for older women, and learning what can be done to prevent that is essential,” she said.

Judith Graham writes a column on aging and health for KFF Health News, where she’s a contributing columnist. She also freelances for other publications. Earlier in her career, Judith contributed more than 80 pieces to the New York Times blog, The New Old Age. She was nominated for a Pulitzer Prize for a series on defective pacemakers and was part of a Chicago Tribune team that won a Pulitzer in 2001.