With this article, journalist Jariel Arvin delves into a complicated situation. The boomers are crowding into their later years at a time when the country has fewer and fewer geriatricians—doctors knowledgeable about their care. Fortunately, the ranks of nurse practitioners trained in geriatrics are growing, but states differ in how much leeway they have to practice independently. KFF Health News posted Arvin’s piece on June 18, 2025. It also ran in the Washington Post. Funding from the Silver Century Foundation helps KFF Health News produce articles (like this one) on longevity and related health and social issues.
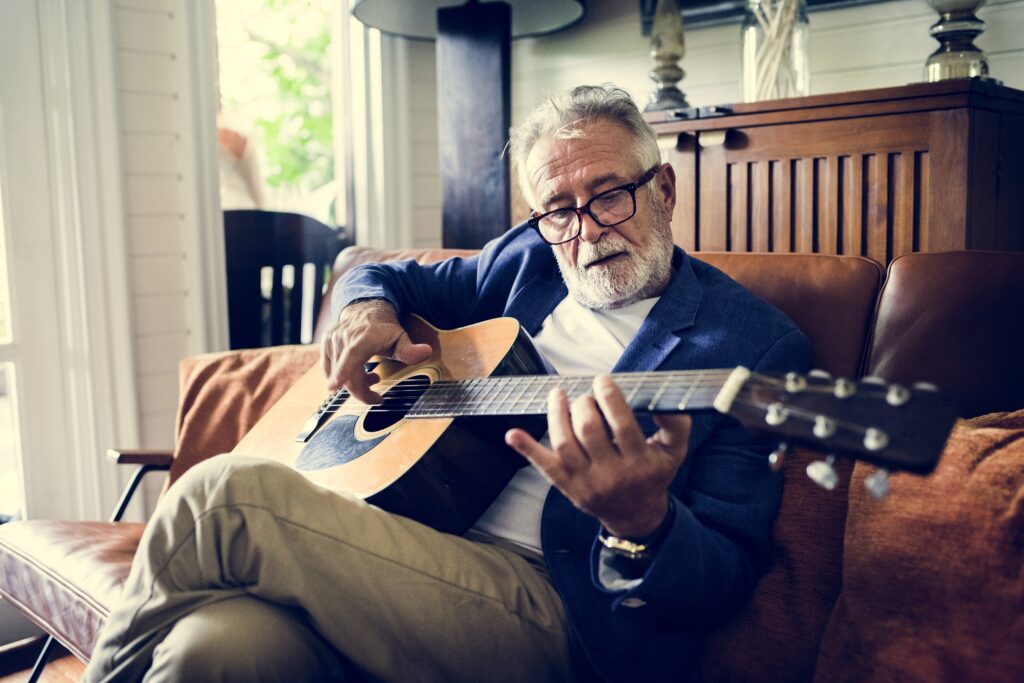
On Fridays, Stephanie Johnson, CRNP, has a busy schedule, driving her navy blue Jeep from one patient’s home to the next, seeing eight in all. Pregnant with her second child, she schleps a backpack instead of a traditional black bag to carry a laptop and essential medical supplies—stethoscope, blood pressure cuff and pulse oximeter.
Forget a lunch break; she often eats a sandwich or some nuts as she heads to her next patient visit.
On a gloomy Friday in January, Johnson, a nurse practitioner who treats older adults, had a hospice consult with Ellen, a patient in her 90s in declining health. To protect Ellen’s identity, KFF Health News is not using her last name.
“Hello. How are you feeling?” Johnson asked as she entered Ellen’s bedroom and inquired about her pain. The blinds were drawn. Ellen was in a wheelchair, wearing a white sweater, gray sweatpants and fuzzy socks. A headband was tied around her white hair. As usual, the TV was playing loudly in the background.
“It’s fine, except this cough I’ve had since junior high,” Ellen said.
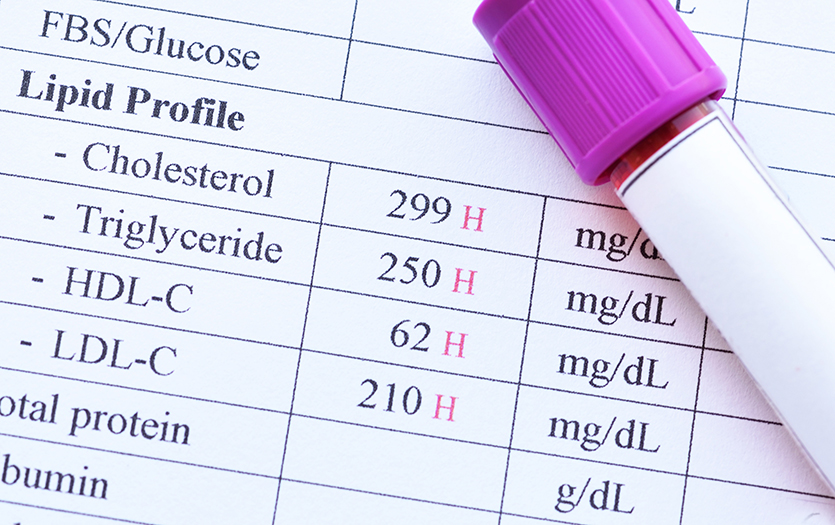
Ellen had been diagnosed with vascular dementia, peripheral vascular disease and Type 2 diabetes. Last fall, doctors made the difficult decision to operate on her foot. Before the surgery, Ellen was always colorful, wearing purple, yellow, blue, pink and chunky necklaces. She enjoyed talking with the half dozen other residents at her adult family home in Washington State. She had a hearty appetite that brought her to the breakfast table early. But lately, her enthusiasm for meals and socializing had waned.
Johnson got down to eye level with Ellen to examine her, assessing her joints and range of motion, checking her blood pressure and listening to her heart and lungs.
Carefully, Johnson removed the bandage to examine Ellen’s toes. Her lower legs were red but cold to the touch, which indicated her condition wasn’t improving. Ellen’s two younger sisters had power of attorney for her and made it clear that, above all, they wanted her to be comfortable. Now, Johnson thought it was time to have that difficult conversation with them about Ellen’s prognosis, recommending her for hospice.
“Our patient isn’t just the older adult,” Johnson said. “It’s also often the family member or the person helping to manage them.”
Nurse practitioners are in a growing occupation, and the number specializing in geriatrics has more than tripled since 2010.
Nurse practitioners are having those conversations more and more as their patient base trends older. They are increasingly filling a gap that is expected to widen as the senior population explodes and the number of geriatricians declines. The Health Resources and Services Administration projects a 50 percent increase in demand for geriatricians from 2018 to 2030, when the entire baby boom generation will be older than 65. By then, hundreds of geriatricians are expected to retire or leave the specialty, reducing their number to fewer than 7,600, with relatively few young doctors joining the field.
That means many older adults will be relying on other primary care physicians, who already can’t keep up with demand, and nurse practitioners, whose ranks are booming. The number of nurse practitioners specializing in geriatrics has more than tripled since 2010, increasing the availability of care to the current population of seniors, a recent study in JAMA Network Open found.
According to a 2024 survey, of the roughly 431,000 licensed nurse practitioners, 15 percent are, like Johnson, certified to treat older adults.
Johnson and her husband, Dustin, operate an NP-led private practice in greater Seattle, Washington, a state, where she can practice independently. She and her team, which includes five additional nurse practitioners, each try to see about 10 patients a day, visiting each one every five to six weeks. Visits typically last 30 minutes to an hour, depending on the case.
“There are so many housebound older adults, and we’re barely reaching them,” Johnson said. “For those still in their private homes, there’s such a huge need.”
Laura Wagner, PhD, a professor of nursing and community health systems at the University of California-San Francisco, stressed that nurse practitioners are not trying to replace doctors; they’re trying to meet patients’ needs, wherever they may be.
“One of the things I’m most proud of is the role of nurse practitioners,” she said. “We step into places where other providers may not, and geriatrics is a prime example of that.”
Practice Limits
Nurse practitioners are registered nurses with advanced training that enables them to diagnose diseases, analyze diagnostic tests and prescribe medicine. Their growth has bolstered primary care, and, like doctors, they can specialize in particular branches of medicine. Johnson, for example, has advanced training in gerontology.
“If we have a geriatrician shortage, then hiring more nurse practitioners trained in geriatrics is an ideal solution,” Wagner said, “but there are a lot of barriers in place.”
In 27 states and Washington, DC, nurse practitioners can practice independently. But in the rest of the country, they need to have a collaborative agreement with or be under the supervision of another health care provider to provide care to older adults. Medicare generally reimburses for nurse practitioner services at 85 percent of the amount it pays physicians.
Last year, in more than 40 states, the American Medical Association and its partners lobbied against what they see as “scope creep” in the expanded roles of nurse practitioners and other health workers. The AMA points out that doctors must have more schooling and significantly more clinical experience than nurse practitioners. While the AMA says physician-led teams keep costs lower, a study published in 2020 in Health Services Research found similar patient outcomes and lower costs for nurse practitioner patients. Other studies, including one published in 2023 in the journal Medical Care Research and Review, have found health care models including nurse practitioners had better outcomes for patients with multiple chronic conditions than teams without an NP.
By 2055, 23 percent of the US population will be 65 or older.
Five states have granted NPs full practice authority since 2021, with Utah the most recent state to remove physician supervision requirements, in 2023. In March, however, Mississippi House Bill 849, which would have increased NP independence, failed. Meanwhile, 30 Texas physicians rallied to tamp down full-scope efforts in Austin.
“I would fully disagree that we’re invading their scope of practice and shouldn’t have full scope of our own,” Johnson said.
She has worked under the supervision of physicians in Pennsylvania and Washington State but started seeing patients at her own practice in 2021. Like many nurse practitioners, she sees her patients in their homes. The first thing she does when she gets a new patient is manage their prescriptions, getting rid of unnecessary medications, especially those with harsh side effects.
She works with the patient and a family member who often has power of attorney. She keeps them informed of subtle changes, such as whether a person was verbal and eating and whether their medical conditions have changed.
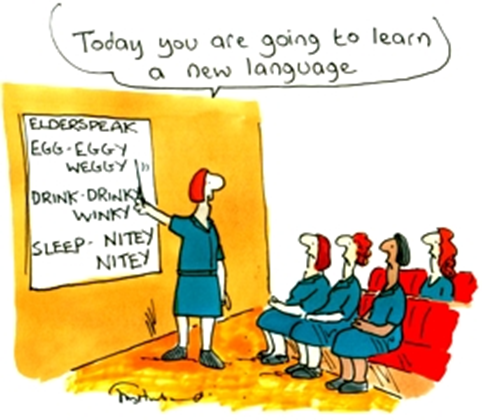
While there is some overlap in expertise between geriatricians and nurse practitioners, there are areas where nurses typically excel, said Elizabeth White, APRN, an assistant professor of health services, policy and practice at Brown University.
“We tend to be a little stronger in care coordination, family and patient education, and integrating care and social and medical needs. That’s very much in the nursing domain,” she said.
That care coordination will become even more critical as the United States ages. Today, about 18 percent of the US population is 65 or over. In the next 30 years, the share of seniors is expected to reach 23 percent, as medical and technological advances enable people to live longer.
Patient and Family
In an office next to Ellen’s bedroom, Johnson called Ellen’s younger sister Margaret Watt to recommend that Ellen enter hospice care. Johnson told her that Ellen had developed pneumonia and her body wasn’t coping.
Watt appreciated that Johnson had kept the family apprised of Ellen’s condition for several years, saying she was a good communicator.
“She was accurate,” Watt said. “What she said would happen, happened.”
A month after the consult, Ellen died peacefully in her sleep.
“I do feel sadness,” Johnson said, “but there’s also a sense of relief that I’ve been with her through her suffering to try to alleviate it, and I’ve helped her meet her and her family’s priorities in that time.”

Jariel Arvin found his way to journalism by an unusual route: after college, he taught English, first in Vietnam and then, with Teach for America, in Oakland, CA. In 2020, he won a fellowship at Vox, a news and opinion website, where he covered the news and wrote a daily newsletter. In 2023, another fellowship brought him to the University of California-Berkeley Graduate School of Journalism, where he’s now a reporter with the Investigative Reporting Program.