Facing her own retirement, journalist Judith Graham contemplates the uncertainties we all face in later life and draws on what she’s learned in four decades as a journalist and more than the eight years writing the “Navigating Aging” column for KFF Health News, which posted this piece on January 15, 2025.
It takes a lot of courage to grow old.
I’ve come to appreciate this after conversations with hundreds of older adults over the past eight years for nearly 200 “Navigating Aging” columns.
Time and again, people have described what it’s like to let go of certainties they once lived with and adjust to new circumstances.
These older adults’ lives are filled with change. They don’t know what the future holds except that the end is nearer than it’s ever been.
And yet, they find ways to adapt. To move forward. To find meaning in their lives. And I find myself resolving to follow this path as I ready myself for retirement.
Patricia Estess, 85, of the Brooklyn borough of New York City spoke eloquently about the unpredictability of later life when I reached out to her as I reported a series of columns on older adults who live alone, sometimes known as “solo agers.”
Estess had taken a course on solo aging. “You realize that other people are in the same boat as you are,” she said when I asked what she had learned. “We’re all dealing with uncertainty.”
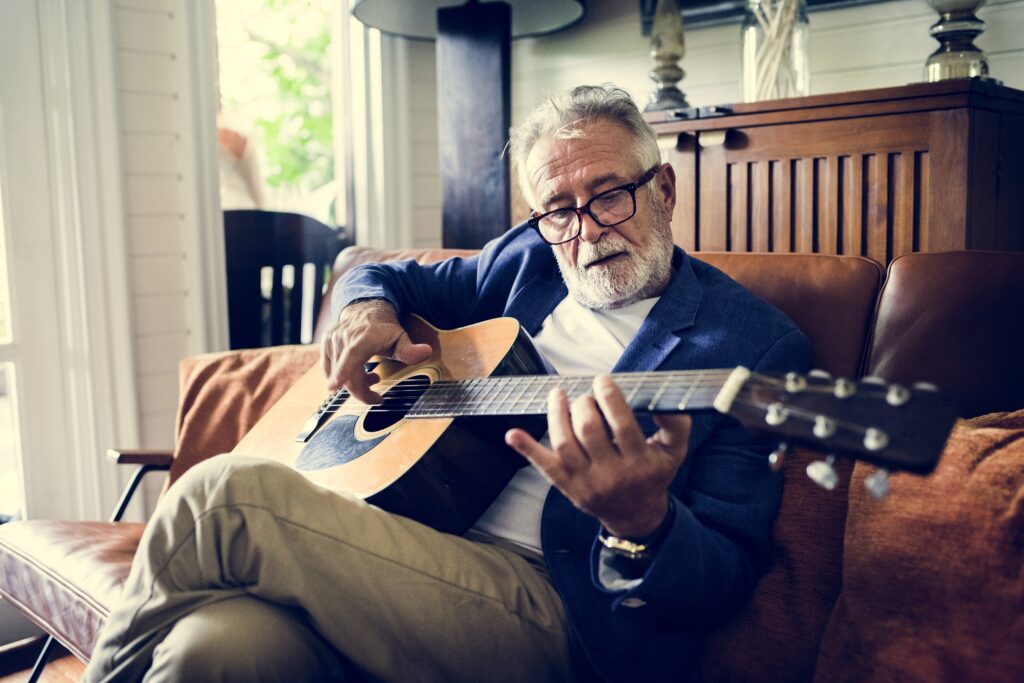
Many people find that embarking on later life changes their sense of identity.
Consider the questions that older adults—whether living with others or by themselves—deal with year in and out: Will my bones break? Will my thinking skills and memory endure? Will I be able to make it up the stairs of my home, where I’m trying to age in place?
Will beloved friends and family members remain an ongoing source of support? If not, who will be around to provide help when it’s needed?
Will I have enough money to support a long and healthy life, if that’s in the cards? Will community and government resources be available, if needed?
It takes courage to face these uncertainties and advance into the unknown with a measure of equanimity.
“It’s a question of attitude,” Estess told me. “I have honed an attitude of, ‘I am getting older. Things will happen. I will do what I can to plan in advance. I will be more careful. But I will deal with things as they come up.’”
For many people, becoming old alters their sense of identity. They feel like strangers to themselves. Their bodies and minds aren’t working as they used to. They don’t feel the sense of control they once felt.
That requires a different type of courage—the courage to embrace and accept their older selves.
Writer May Sarton described old age as ‘a foreign country with an unknown language.’
Marna Clarke, a photographer, spent more than a dozen years documenting her changing body and her life with her partner as they grew older. Along the way, she learned to view aging with new eyes.
“Now, I think there’s a beauty that comes out of people when they accept who they are,” she told me in 2022 when she was 82, just before her 93-year-old husband died.
Arthur Kleinman, a Harvard professor who’s now 83, gained a deeper sense of soulfulness after caring for his beloved wife, who had dementia and eventually died, leaving him grief-stricken.
“We endure, we learn how to endure, how to keep going. We’re marked, we’re injured, we’re wounded. We’re changed, in my case for the better,” he told me when I interviewed him in 2019. He was referring to a newfound sense of vulnerability and empathy he gained as a caregiver.
Herbert Brown, 68, who lives in one of Chicago’s poorest neighborhoods, was philosophical when I met him at his apartment building’s annual barbecue in June.
“I was a very wild person in my youth. I’m surprised I’ve lived this long,” he said. “I never planned on being a senior. I thought I’d die before that happened.”
Truthfully, no one is ever prepared to grow old, including me. (I’m turning 70 in February.)
Chalk it up to denial or the limits of imagination. As May Sarton, a writer who thought deeply about aging, put it so well, old age is “a foreign country with an unknown language.” I, along with all my similarly aged friends, are surprised we’ve arrived at this destination.
I’ve come to see that ‘no guarantees’ isn’t a reason to dig in my heels and resist change.
— Judith Graham
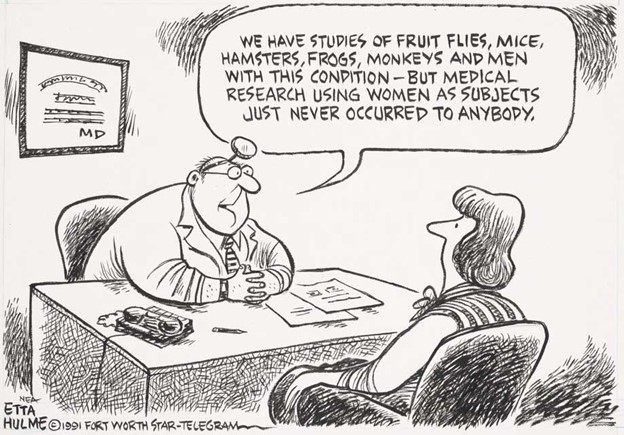
For me, 2025 is a turning point. I’m retiring after four decades as a journalist. Most of that time, I’ve written about our nation’s enormously complex health care system. For the past eight years, I’ve focused on the unprecedented growth of the older population—the most significant demographic trend of our time—and its many implications.
In some ways, I’m ready for the challenges that lie ahead. In many ways, I’m not.
The biggest unknown is what will happen to my vision. I have moderate macular degeneration in both eyes. Last year, I lost central vision in my right eye. How long will my left eye pick up the slack? What will happen when that eye deteriorates?
Like many people, I’m hoping scientific advances outpace the progression of my condition. But I’m not counting on it. Realistically, I have to plan for a future in which I might become partially blind.
It’ll take courage to deal with that.
Then, there’s the matter of my four-story Denver house, where I’ve lived for 33 years. Climbing the stairs has helped keep me in shape. But that won’t be possible if my vision becomes worse.
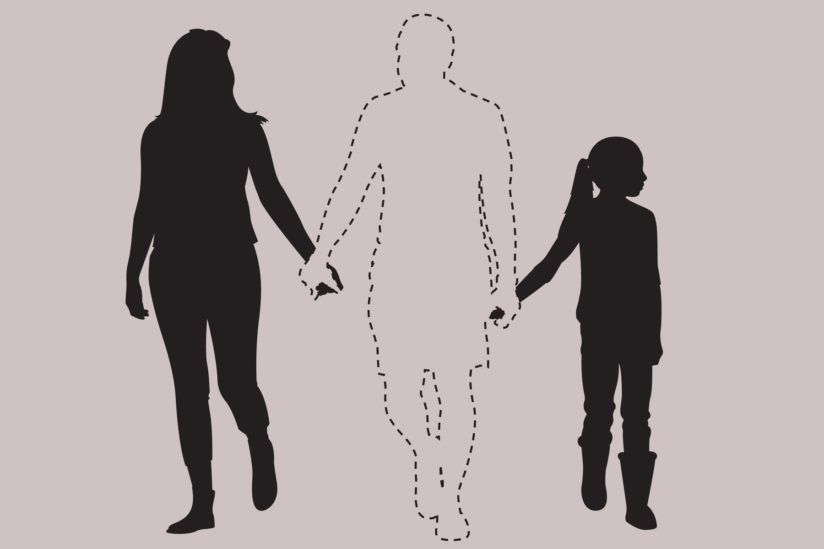
So my husband and I are taking a leap into the unknown. We’re renovating the house, installing an elevator and inviting our son, daughter-in-law and grandson to move in with us. Going intergenerational. Giving up privacy. In exchange, we hope our home will be full of mutual assistance and love.
There are no guarantees this will work. But we’re giving it a shot.
Without all the conversations I’ve had over all these years, I might not have been up for it. But I’ve come to see that “no guarantees” isn’t a reason to dig in my heels and resist change.
Thank you to everyone who has taken time to share your experiences and insights about aging. Thank you for your openness, honesty and courage. These conversations will become even more important in the years ahead, as baby boomers like me make their way through their 70s, 80s and beyond. May the conversations continue.

Judith Graham writes a column on aging and health for KFF Health News, where she’s a contributing columnist. She also freelances for other publications. Earlier in her career, Judith contributed more than 80 pieces to the New York Times blog, The New Old Age. She was nominated for a Pulitzer Prize for a series on defective pacemakers and was part of a Chicago Tribune team that won a Pulitzer in 2001.